Conference discusses latest updates on female sexual dysfunction treatment
Society – Economy - Ngày đăng : 11:24, 31/10/2024
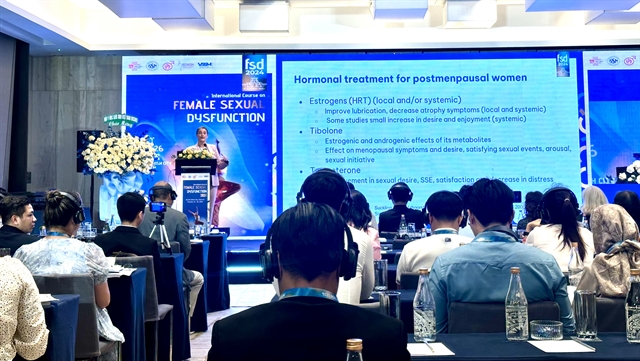 |
| An international course on female sexual dysfunction was organised at Bình Dân Hospital in HCM City from October 25 to 26. — VNS Photo Nguyễn Diệp |
HCM CITY — Female sexual dysfunction (FSD) has a negative impact not only on women's physical and mental health, but also on their marital relationship quality and quality of life, attendees heard at a two-day international course held in HCM City.
The course was organised from October 25 to 26 by the HCM City-based Bình Dân Hospital in collaboration with the International Society for Sexual Medicine (ISSM), International Society for the Study of Women's Sexual Health (ISSWSH), Asia Pacific Society for Sexual Medicine (APSSM) and Vietnam Society for Sexual Medicine (VSSM).
Speaking at the event, Trần Vĩnh Hưng, director of Bình Dân Hospital, said the course was organised for the first time in Việt Nam to share knowledge and information on healthcare issues relating to female sexual dysfunction.
“It provides doctors specialising in obstetrics and gynecology, urology, andrology, endocrinology, aesthetics, psychology and sociology an overview of female sexual dysfunction, and updates criteria for diagnosis and treatment,” he said.
The conference was carried out by professors from the US, Europe (Italy, Germany and Denmark) and Asia (The Republic of Korea), along with leading domestic speakers.
Approximately 40-50 per cent of women of all ages reported at least one sexual dysfunction, according to the consensus of the 4th International Consultation on Sexual Medicine (ICSM) held in 2015.
The results from a global study of 27,500 people (about half of whom were women aged 40 - 80 years) showed that a large proportion of women experienced multiple sexual dysfunctions, with 17 per cent in Northern Europe and 34 per cent in Southeast Asia.
Women with psychosis often have problems with arousal, delayed or no orgasm, less sexual activity, and lower sexual satisfaction.
New research shows that sexual desire might not be affected much by psychosis.
Causes of sexual problems include medications, symptoms of psychosis (both positive and negative), difficulties with relationships, stigma, and time spent in institutions.
Women with psychosis often say the "lack of a partner" is a reason for low sexual satisfaction, PhD Julia Velten, a clinical psychologist, cognitive-behavioral therapist and sex therapist, said.
“Internalised stigma makes it harder for women to form close relationships,” she said.
About 65 per cent of women with psychotic disorders have very low sexual self-esteem (compared to 29 per cent of healthy women).
Physical issues like metabolic syndrome, acne, side effects from medications (extrapyramidal symptoms), and breast milk leakage can also cause sexual problems.
Mental disorders are common and are strongly linked to sexual problems in women.
“Having mental health issues can make it harder to diagnose and treat sexual problems,” she said.
Sexual problems can cause women to stop taking their prescribed medications (non-compliance).
When a woman has sexual problems, they should always check if these issues are connected to any other major mental health conditions, she noted.
“When a woman seeks treatment for a mental disorder like depression, anxiety, or PTSD, check if the disorder or its medication is causing serious sexual problems.”
 |
| The two-day international course provided an overview of female sexual dysfunction, and updated criteria for diagnosis and treatment. — VNS Photo Nguyễn Diệp |
Annamaria Giraldi, editor-in-chief for sexual medicine reviews at ISSM, discussed how to conduct an interview about sexual dysfunction.
“A questionnaire is never a substitute for a clinical interview,” she said.
Barriers for the sexual health interview include taboos; fear of embarrassing the patient; being embarrassed yourself; lack of time, privacy in the consultation, language, and knowledge about the problem and treatment; and clinicians believing, “it's not so important for the patient" and “If they have problems, they will tell me.”
A interview should be in four steps: elicit the patient’s story, name and (re)frame attention to sexual concerns or problems, empathic witnessing, and referral, or assessment and treatment.
She also introduced the PLISSIT (Permission, Limited Information, Specific Suggestion, Intensive Therapy) model.
“The model gives patients permission to raise sexual issues and limited information about sexual problems and treatments,” she said.
It also makes specific suggestions based on the assessment of the problem, and refers to or initiates more intensive therapy like sex therapy, specialised medical therapy and psychotherapy, she added.
The need for sexual counseling is a reality. More activities are needed to raise awareness on sexual health care, Ngô Thị Yên of the sexual counseling unit of Từ Dũ Hospital in HCM City said.
The unit’s data in 2023 showed that all of six domains of FSD (desire, arousal, lubrication, orgasm, satisfaction and pain) are still at high rates.
Outstanding factors include lack of knowledge on the sexual response cycle, stressful job/life and a lack of open talk with husbands about sexuality, she said.
Successful treatments for women are thanks to tools for diagnosis, medical staff paying more attention, protocols for intervention, and clients’ awareness.
Associate Professor Tami Serene Rowen of Obstetric, Gynecology and Reproductive at the University of California said no single treatment is ideal for every woman.
“Do not forget to do a thorough physical exam,” she said.
It is crucial to keep in mind the biopsychosocial model of FSD.
Nearly all women with any long-term pain will have a significant psychological component that needs to be addressed.
Many common obstetric and gynecologic conditions can affect sexual health.
“It’s important to consider the effects on sex and relationships and to address this in the clinic.”
When counseling patients on treatments for their conditions, please consider the effects on sexual health and provide anticipatory guidance and explanations so they are aware there may in fact be an effect on their sexual health. — VNS
